Recent Findings Advance our Understanding of How Frontline Employees Contribute to Patient Adherence in Mental Healthcare
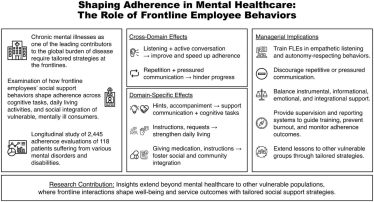
A new study by Victoria Kramer, Janina Wiebringhaus, Detelina Marinova, and Manfred Krafft—published in the Journal of Service Research as part of a special issue on disadvantaged and vulnerable consumers—sheds light on a question in mental healthcare and service research that remains insufficiently understood: How do everyday interactions between frontline employees and patients shape adherence and well-being?
With chronic mental illnesses affecting more than one billion people worldwide, and treatment costs projected to rise substantially in the coming years, the need for effective, person‑centered service delivery has become a societal priority. Individuals living with chronic mental illnesses or intellectual disabilities often face cognitive, emotional, and behavioral challenges that make them especially vulnerable in service settings. For healthcare systems, this vulnerability translates into a critical responsibility: ensuring that patients can follow treatment plans, engage in daily tasks, and work toward greater independence.
Why Frontline Interactions Matter
Frontline employees (FLEs) are the professionals who interact most frequently and directly with patients—supporting medication routines, guiding daily activities, and helping individuals navigate social and community life. Yet, despite their central role, little empirical evidence exists on which FLE behaviors actually help patients adhere to treatment recommendations, especially in mental healthcare.
This study fills that gap by analyzing a rich, longitudinal dataset from a large healthcare organization. Drawing on social support theory, the researchers examined how specific FLE behaviors—such as ensuring, reminding, reflecting, and accompanying—affect adherence across multiple domains, from communication skills to daily living tasks and broader social integration.
Key Findings: Listening Helps, Repetition Hurts
The results underscore the importance of active, engaged communication. Behaviors that involve fostering genuine dialogue as well as listening carefully and reflecting on patients’ experiences significantly increase both the likelihood and speed of adherence improvements.
In contrast, repetitive or disengaged behaviors—such as mechanically reminding patients without meaningful interaction—can reduce adherence likelihood by more than five percent and slow progress over time.
These insights suggest that effective support in mental healthcare is not just about what FLEs do, but also how they do it.
Implications for Practice
For healthcare organizations, the findings imply that investing in the micro‑behaviors of frontline staff can yield meaningful improvements in patient outcomes. Training programs that emphasize empathetic communication, reflective dialogue, and adaptive support strategies can help create more dignified, responsive, and effective care environments.
While the study focuses on mental healthcare, its insights extend to other vulnerable groups, including the elderly, individuals with chronic physical conditions, and those facing socioeconomic hardship. In all these settings, person‑centered frontline behaviors are key to fostering autonomy, stability, and well-being.
Read the full article here: https://journals.sagepub.com/doi/10.1177/10946705251410017

